This is one in a series of articles that provide detailed and updated information about Dental Bone Graft.
In this specific article, which focuses on Dental Bone Graft – Overview, you can read about:
For additional articles about Dental Bone Graft, see the Topic Menu.
What is a dental bone graft?
A dental bone graft addresses the common issue of insufficient bone quantity often encountered in routine dentistry. Bone resorption or the development of ridge defects may occur due to factors such as age, infection, trauma, surgery, or congenital malformations. The primary cause of bone loss is the lack of intraosseous stimulation. As a result, the main goal of a dental bone graft is to promote bone formation, maintain the newly formed bone, preserve contours, eliminate dead space, and minimize postoperative infection. In essence, a dental bone graft is a material that enhances the healing of both bony and soft tissues.
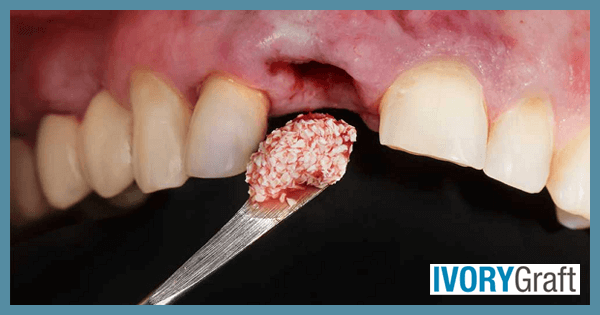
Tooth loss, which may be attributed to age-related factors or surgical removal, is a major contributor to bone resorption, due to the absence of intraosseous stimulation provided by the periodontal ligament. Dental bone grafts can help prevent resorption by increasing volume and density in areas where bone loss has occurred. The graft material can be sourced from the patient’s body (autogenous), a human tissue bank (allograft), an animal tissue bank (xenograft), or, in some cases, be synthetic (alloplastic).
The bone graft placement procedure involves these steps:
- Identifying the appropriate site for bone graft placement.
- Using local anesthesia to numb the site in preparation for surgery.
- Making a small incision in the gums and retracting the gum tissue to visualize the alveolar bone.
- Thoroughly cleaning and disinfecting the defective area on the alveolar bone, then placing the bone grafting material onto it.
- Typically, a separating membrane is placed between the gum tissue and the bone graft to protect the graft and provide more space for bone regeneration.
- Repositioning the gum tissue onto the membrane and closing the incision with stitches.
After the surgery, patients receive post-operative instructions that address the expected pain, swelling, and bruising that may last for a few days. To prevent infections and alleviate pain symptoms, antibiotics and painkillers are prescribed.
What do dental bone grafts do?
Dental bone grafts play a vital role when a tooth is lost or extracted. The alveolar bone, an important supportive component, begins to deteriorate or shrink over time due to the loss of the periodontal ligament, which is the major source of stimulation for bone formation. In such scenarios, it becomes challenging to place a prosthesis or implant necessary for functionality or aesthetics.
Tooth replacement procedures, like dental implants, require sufficient volume and density of bone to ensure proper anchorage. Dental bone grafts help restore bone in cases of resorbed ridges, providing stable support for dental implants or other prostheses used for tooth replacement. Without a bone graft, the implant or prosthesis may not be stable enough to support chewing or biting forces, which can lead to treatment failure.
How dental bone graft works?
Bone graft placement surgery involves placing a graft into the area where the bone has deteriorated. The bone graft material promotes bone regeneration, which, over time, fuses with the existing bone and provides stable support for the dental implant or other tooth replacement prostheses. The process of bone integration can take several months, and once enough bone is available, the implant or prosthesis can be placed.
Dental bone grafts serve as a scaffold for new bone formation or regeneration. The biologic mechanisms that provide a rationale for bone grafting are osteoconduction, osteoinduction, osteopromotion, and osteogenesis.
- Osteoconduction: the process by which a bone graft material acts as a scaffold for new bone formation, which is the minimal required function of a bone graft. During this process, osteoblasts, the bone-forming cells, migrate from the margin of the bony defect to the graft material, which serves as a framework. As the osteoblasts accumulate on this framework, they start to spread and generate new bone, thereby facilitating the integration of the graft material with the existing bone.
- Osteoinduction: the process that involves the stimulation of osteoprogenitor cells to differentiate into osteoblasts, which are responsible for new bone formation. An osteoinductive bone graft material not only serves as a scaffold for osteoblasts but also triggers the formation of new osteoblasts, ultimately enhancing the entire bone regeneration process. This mechanism is essential for the successful integration of bone grafts and the restoration of bone defects.
- Osteopromotion: the enhancement of osteoinduction without directly participating in bone formation. This process involves the use of certain factors or substances that can improve the bone regeneration process by promoting the activity of osteoinductive agents. Osteopromoters, such as platelet-rich plasma (PRP) taken from the patient’s blood, can accelerate and improve the quality of bone healing by stimulating the activity of osteoblasts and other bone-forming cells.
- Osteogenesis: the process of new bone formation by osteoblasts. It involves the synthesis and deposition of bone matrix, which eventually mineralizes to form mature bone tissue. Osteogenesis is a crucial aspect of bone grafting, as it ensures that the graft material successfully integrates with the existing bone and provides the necessary support and stability for dental implants or other tooth replacement prostheses.
To summarize, the best dental bone grafts work by attracting and hosting osteoblasts (= Osteoconduction), inducing the creation of new osteoblasts (= Osteoinduction) and promoting it (=Osteopromotion), and therefore encouraging new bone development (=Osteogenesis).
Are dental bone grafts necessary?
A dental bone graft is placed in a specific area on the alveolar bone when the quantity and quality of the bone are inadequate. It is primarily used to support dental implants or other prostheses needed for missing teeth, as well as in surgeries such as periodontal surgery to correct bone defects caused by periodontal disease, third molar removal, or excision of bony lesions.
The necessity of a dental bone graft depends on the specific needs of each case and the treatment plan. Each patient can be evaluated to determine whether a bone graft is required or not.
For example, in situations where there is significant bone loss, a dental bone graft may be necessary to ensure the success of a dental implant by providing better stability and support. In cases where a tooth has been lost or severely weakened due to gum disease, a bone graft may be needed to provide additional support for the remaining teeth. Without a bone graft, the surrounding teeth may shift or become loose, leading to further dental problems.
When is dental bone grafting necessary?
Bone loss can occur due to tooth loss, aging, periodontal disease, or trauma. Dental bone grafting can be used to restore or increase the amount of bone in the jaw lost as a result of these factors.
Some common situations where bone grafting may be necessary include:
- In cases of multiple missing teeth, where tooth replacement can only be accomplished with the help of an implant, sufficient bone support is needed for the implant to be successful. Bone grafting becomes crucial in these cases, as it helps build up the alveolar bone, enabling the implant to be placed.
- In cases of periodontal disease with significant bone loss, a dental bone graft can be used to augment the alveolar bone and provide better stability to the teeth affected by bone loss, leading to an overall improvement in prognosis.
- For the fabrication of dentures in elderly patients with severe bone loss, ridge augmentation using a dental bone graft can be considered to provide better retention and stability for the dentures.
- After a traumatic injury to the jaw where bone damage has occurred, a bone graft can be used to repair the damage and restore the alveolar bone both functionally and aesthetically.
Dental bone graft benefits
The primary purpose of a dental bone graft is to enhance the quality and quantity of alveolar bone, which can lead to the following benefits:
- For replacing missing teeth, any procedure requires adequate bone support. Dental implants are the most popular method for tooth replacement, but they necessitate a sufficient amount of alveolar bone for a successful outcome. Bone grafting can be highly beneficial in cases where an implant is needed and bone support is inadequate.
- Bone grafting can be extremely advantageous when periodontal treatment is required. Teeth without proper bone support are at risk of exfoliation. Bone grafting can be employed to rebuild the alveolar bone and provide the necessary support to preserve natural teeth affected by bone loss.
- It is a natural occurrence that some bone loss is observed following tooth loss, whether due to extraction or natural causes. To prevent this, a bone graft can be used after extraction, especially after third molar surgery, to benefit the remaining bone and avoid further loss of alveolar bone.
Dental bone grafting can offer numerous advantages for patients, from improving oral function to boosting self-confidence and preventing future dental issues. A dental professional can evaluate a patient’s specific needs and determine if bone grafting is an appropriate option.
Bone graft for tooth implant
A dental implant has a specific macro design that demands certain dimensional properties from the bone for its success. Implant placement requires sufficient bone volume and good biological quality. Before implant placement, the following bone conditions are considered:
- Soft tissue follows hard tissue, so before implant planning in an esthetic area, the bony base must be evaluated for functional and esthetic success.
- Post-extraction, there is some resorption of the edentulous ridge which must be assessed. A bone graft can then be used for vertical augmentation of the mandible and maxilla or horizontal augmentation of the mandible and maxilla.
- Presence of any infection or bony defects due to trauma should be considered.
- The bone graft can be used to fill empty spaces in the bone in cases of peri-implantitis.
Selecting an appropriate surgical technique and graft material is crucial. A bone graft may fail to integrate if proper planning or execution is not carried out, which may result in the resorption of the graft material. Consequently, the lost tissue may be replaced with fibrous tissue rather than functional bone.
Dental bone graft without implant
Typically, a bone graft is considered when an implant is anticipated to provide proper support. However, it can also be performed without an implant in cases where ridge preservation is needed, or post-surgery correction is required. A bone graft, which can be a small piece of bone taken from another part of the patient’s body or a synthetic material, is used to augment or replace bone that has been lost due to injury, disease, or tooth extraction.
After the surgery, during the healing or integration phase of the graft, the patient is advised not to chew on hard foods for several weeks and to maintain proper oral hygiene to ensure the best possible outcome. When a bone graft is placed without an implant, it can be used to promote bone growth and regeneration, which helps maintain the integrity of the jawbone and prevents further deterioration.
Dental bone graft for dentures
Dentures are designed for edentulous ridges, which are at the highest risk of resorption. In most cases involving dentures, a bone graft is seldom considered but is strongly recommended. After tooth extraction, there is a significant chance of bone loss, and dentures given in such cases may become loose over time. For proper retention and comfort, a denture should compress uniformly against the gum, with a smooth ridge and no sharp bony areas.
During extraction, it is advised to reduce and smooth the ridge for future treatment protocols. However, in some cases, even after following routine procedures, the denture may lose its stability and retention over time. If bone grafts are used before denture fabrication, a better surface for the denture to sit on can be provided, preventing problems with stability. The use of bone grafts slows bone resorption compared to the normal rate. While implants can be an excellent option for denture retention, their cost is significantly higher than bone grafts..
Dental bone graft for bridge
Shrunken and resorbed ridges can make fitting a removable appliance difficult. A bone graft can be beneficial for placing a bridge over an edentulous site, as it prevents tissue resorption over time, which would otherwise create a space between the ridge and the bridge. For posterior bridges, the main issue is food impaction, which can further worsen the situation. In cases of anterior bridges, resorbed ridges can result in an unsightly black space beneath the bridge.
Using a bone graft at the time of extraction can prevent resorption and, consequently, the failure of a dental bridge in terms of both functionality and aesthetics.
Dental bone graft for bone loss
As age advances, osteoporosis increases, leading to thin alveolar ridges due to bone loss. Loss of bone mass in the jaw can cause the face to appear shorter, impacting an individual’s appearance. This reduction in the vertical height of the face is also associated with changes in facial profile, lip and muscle appearance, and increased skin wrinkling in the jaw area, particularly when bone loss occurs in the lower jawbone and habitual chewing leads to protrusion.
Bone grafting can offer a solution to these aesthetic problems, improving not only the functional aspect of the oral and maxillofacial complex but also the overall aesthetics. Bone grafts are especially important in cases where significant bone loss occurs after treatment of large jaw lesions or extensive traumatic injuries.
In cases of temporomandibular joint (TMJ) abnormalities, such as agenesis or fusion of TMJ bones, bone grafting serves as the best treatment option.


