This is one in a series of articles that provide detailed and updated information about Dental Bone Graft.
In this specific article, which focuses on Dental Bone Graft – Accessories and additives, you can read about:
For additional articles about Dental Bone Graft, see the Topic Menu.
Dental bone graft kit
A dental bone graft is a critical procedure, and its success depends on various factors, including the use of proper equipment and adherence to the correct protocol. Dental bone graft kits are designed to provide all necessary materials and instruments in one convenient package, ensuring efficiency and effectiveness in performing the procedure.
A dental bone graft kit is a set of specialized instruments and materials used in dental procedures for bone grafting. The specific contents of a dental bone graft kit can vary depending on the procedure being performed and the preferences of the dentist or oral surgeon.
Typically, the kit includes bone grafting materials, such as bone graft granules or bone graft putty, as well as instruments like drills, curettes, and scalpel blades. Some kits may also feature dental bone graft mesh, which offers additional support for the bone graft material. Dental bone graft kits are employed in various procedures, including ridge augmentation, sinus lifts, and guided bone regeneration.
Dental bone graft with membrane
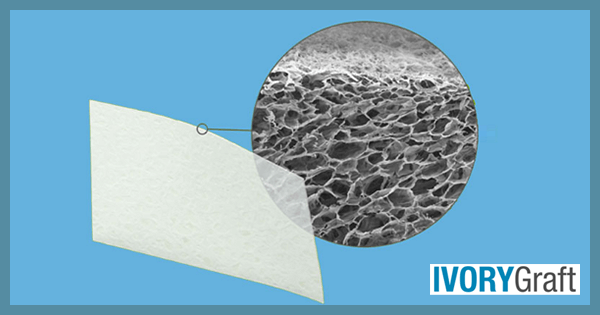
A dental bone graft with a membrane involves using a thin, specialized membrane to protect and support the graft during the healing process. The membrane acts as a barrier to prevent unwanted tissue from growing into the graft site while allowing bone cells and nutrients to pass through and promote bone growth.
Membrane types and characteristics:
- Resorbable VS non-resorbable membranes:
-
- Resorbable membranes are made of collagen products that dissolve in the body over time, with most being xenoplastic (from animals).
- Non-resorbable membranes do not dissolve and generally need to be removed after a fixed time.
- Synthetic VS biologic membranes:
-
- Synthetic membranes are made from polytetrafluoroethylene (PTFE), such as Gore-Tex, and can have a moldable titanium layer within them to act as a mesh for providing shape to the graft.
- Biological membranes are derived from blood, such as platelet-rich plasma (PRP), platelet-rich fibrin (PRF), or concentrated growth factors (CGF). Some blood components are mixed with grafting materials to create autologous fibrin glue (AFG).
Here are the steps involved in a dental bone graft with a membrane:
- Anesthesia: The patient is given local anesthesia to numb the area where the bone graft will be placed.
- Incision: A small incision is made in the gum tissue to expose the area where the bone graft will be placed.
- Preparation of the graft material: The bone graft material is prepared and shaped to fit the area where the bone needs to be added.
- Placement of the graft: The bone graft material is placed into the area where the bone is needed and secured in place using specialized instruments.
- Placement of the membrane: The membrane is placed over the bone graft material, covering the entire graft site.
- Closure: The incision in the gum tissue is closed using stitches.
- Recovery: The patient follows specific post-operative care instructions, including avoiding certain foods and activities, and attending follow-up appointments with their dental professional to monitor the healing process.
The use of a membrane in a dental bone graft can improve the success rate of the procedure by providing additional support and protection to the bone graft material during the healing process.
Dental bone graft with plasma
A dental bone graft with plasma involves using platelet-rich plasma (PRP) to aid in the healing process of the bone graft. Plasma is a by-product of blood that is rich in platelets, which can greatly accelerate the rate of normal healing. Platelets perform many functions, including blood clot formation and the release of growth factors (GF) into the wound, stimulating stem cells to regenerate new tissue. These growth factors include platelet-derived growth factors (PDGF), transforming growth factor beta (TGF), insulin-like growth factor (ILGF), and bone morphogenic protein (BMP), which can induce the formation of new bone. By adding PRP and BMP to the bone graft, new bone can grow faster.
Here are the steps involved in a dental bone graft with plasma:
- Blood draw: A small amount of the patient’s blood is drawn.
- PRP preparation: The blood is processed to concentrate the platelets and growth factors into a small amount of plasma.
- Anesthesia: The patient is given local anesthesia to numb the area where the bone graft will be placed.
- Incision: A small incision is made in the gum tissue to expose the area where the bone graft will be placed.
- Preparation of the graft material: The bone graft material is prepared and shaped to fit the area where the bone needs to be added.
- Application of PRP: The PRP is applied to the bone graft material, coating it with a layer of concentrated platelets and growth factors.
- Placement of the graft: The bone graft material, now coated with PRP, is placed in the area where the bone is needed.
- Closure: The incision in the gum tissue is closed using stitches.
- Recovery: The patient follows specific post-operative care instructions, including avoiding certain foods and activities, and attending follow-up appointments with their dental professional to monitor the healing process.
The use of PRP in a dental bone graft can improve the success rate of the procedure by promoting tissue regeneration and accelerating the healing process.
Dental bone graft with blood
The patient’s blood can be used as a source of growth factors. As discussed above plasma is the by-product of blood that is rich in platelets. The blood is typically drawn from the patient just before the bone graft procedure and processed to obtain a concentration of growth factors known as platelet-rich plasma (PRP) or platelet-rich fibrin (PRF). A dental bone graft with blood involves the use of PRP to accelerate the healing process of the bone graft.
Here are the steps involved in a dental bone graft with blood:
Blood draw: A small amount of the patient’s blood is drawn just before the bone graft procedure.
PRP or PRF preparation: The blood is then processed to obtain a concentrate of growth factors, either PRP or PRF.
Anesthesia: The patient is given local anesthesia to numb the area where the bone graft will be placed.
Incision: A small incision is made in the gum tissue to expose the area where the bone graft will be placed.
Preparation of the graft material: The bone graft material is prepared and shaped to fit the area where the bone needs to be added.
Mixing of blood concentrate with bone graft: The PRP or PRF is mixed with the bone graft material.
Placement of the graft: The bone graft material, now mixed with PRP or PRF, is placed in the area where the bone is needed.
Closure: The incision in the gum tissue is closed using stitches.
Recovery: The patient will need to follow specific post-operative care instructions, including avoiding certain foods and activities, and attending follow-up appointments with their dental professional to monitor the healing process.
The use of the patient’s blood in a dental bone graft can improve the success rate of the procedure by providing a concentrated source of growth factors to aid in tissue regeneration and accelerate the healing process.
Dental bone graft and blood donation
After a dental bone graft procedure, there is some amount of blood loss that can be critical from a blood donation perspective. Patients may need to wait at least 72 hours before donating blood to ensure they have fully recovered from surgery and there is no risk of bleeding or infection. It’s important to inform the blood donation center staff about any recent dental procedures, including bone grafting, before donating blood. This ensures the blood is safe for the recipient and that the donor is not at risk of any complications.
The length of time for recovery also depends on the type of bone graft used, the amount of blood loss during the procedure, and the individual’s overall health.
In some cases, blood donation is prohibited after bone graft surgery, such as when platelet-rich plasma (PRP) or platelet-rich fibrin (PRF) is used with the bone graft. The use of these blood concentrates may increase the concentration of platelets, causing faster blood clotting and making the blood unsuitable for donation.
Dental bone graft sutures
During a dental bone grafting procedure, an incision is made in the gum, to access the site where the graft needs to be placed. Once the process is complete, the incision is closed with sutures (threads for closing a wound). The type of sutures used depends on the specific needs of the patient and the complexity of the procedure.
Sutures can be either dissolvable or non-dissolvable. In most cases, dissolvable sutures are used for dental bone grafts. These sutures are made of materials that break down over time and are absorbed by the body, eliminating the need for removal. Dissolvable sutures are typically used for procedures requiring minimal support or closure.
For more complex procedures that require greater support or closure, non-dissolvable sutures may be used. These sutures are made of materials such as silk, nylon, or polypropylene and must be removed by the dentist or oral surgeon after the incision has healed.
Proper healing of the graft depends on maintaining a clean and intact surgical site. Sutures provide support, keeping the bone graft in place and ensuring the wound remains closed. This creates a clean and secure environment, which can further enhance healing.
Do dental bone grafts require stitches?
During a dental bone grafting procedure, an incision is made in the gum to access the site where the graft must be placed. Once the process is complete, the incision is closed with stitches. The type of stitches, or sutures, used depends on the patient’s specific needs and the complexity of the procedure.
Sutures may be dissolvable or non-dissolvable. In most cases, dissolvable sutures are used for dental bone grafts. These sutures are made of materials that break down over time and are absorbed by the body, eliminating the need for removal. Dissolvable sutures are typically used for procedures requiring minimal support or closure.
For more complex procedures that demand greater support or closure, non-dissolvable stitches may be employed. These sutures are made of materials such as silk, nylon, or polypropylene and must be removed by the dentist or oral surgeon once the incision has healed.
Proper healing of the graft requires the surgical site to remain clean and intact. Stitches provide support to keep the bone graft in place and the wound closed, which further enhances healing by maintaining a clean and secure environment.
Dental bone graft using stem cells
Dental bone grafts using stem cells are a relatively new technology, and further research is needed to determine their long-term effectiveness and safety. Stem cells, typically obtained from the patient’s bone marrow or a donor source, can differentiate into various cell types, including bone cells (osteoblasts).
After extracting the stem cells, they are concentrated and combined with a scaffold material, such as collagen or hydroxyapatite. This combination is then placed at the site of the bone graft. These stem cells differentiate into bone cells, stimulating the growth of new bone tissue. This process can potentially lead to faster healing and improved outcomes compared to traditional bone graft procedures.
It is important to note that not all bone grafts can be used with stem cells. The decision to use a dental bone graft with stem cells should be carefully considered based on the patient’s needs and medical history. Additionally, the cost of this procedure may be higher than traditional bone grafts, as it involves advanced technology and specialized equipment.
Dental bone graft and X-ray
X-rays play a crucial role in the assessment of dental bone grafts. They are used to evaluate the grafts before, during, and after the procedure. Various imaging modalities can be employed to assess the jawbone’s condition and monitor the healing process, based on the number of surgical sites where grafting is performed.
Dental imaging related to bone grafting may include the following scan:
- Before grafting: Initially, a standard IOPA (Intra-Oral Periapical Radiograph) can be conducted for evaluation purposes. If bone grafting is required due to bone loss, 3D imaging such as CBCT can be performed to calculate the quality and quantity of the remaining alveolar bone, allowing for proper grafting procedure planning. Imaging also helps evaluate other vital structures, such as the position of the maxillary sinus, IANC (inferior alveolar nerve canal), mental foramen and adjacent teeth, before placing the graft.
- During grafting: During the procedure, x-rays may be utilized to ensure that the graft material is placed correctly and fully integrated with the surrounding bone tissue. Any signs of infection, bone graft resorption, or improper healing can be identified, appearing as radiolucency within or around the graft.
- After grafting: After the bone graft procedure, follow-up x-rays may be taken to monitor the healing process and ensure that the graft material is being incorporated into the existing bone tissue. This helps assess the success of the grafting procedure and determine if any additional treatment is needed.
X-rays are an effective way to evaluate the condition of the alveolar bone and monitor the healing process after a dental bone graft. However, it is important to minimize unnecessary radiation exposure and use x-rays only when necessary and unavoidable for evaluation and treatment planning.


