This is one in a series of articles that provide detailed and updated information about Dentin.
In this specific article, which focuses on Dentin – Growth and Formation, you can read about:
For additional articles about Dentin, see the Topic Menu.
Dentin growth
Dentin is a hard, mineralized vital tissue that is formed by specialized cells called odontoblasts. dentin makes up the bulk of a tooth. Odontoblast is located in the pulp of the tooth. Throughout life, the growth of dentin occurs continuously, as the odontoblasts lay down new layers of dentin on the inner surface of the existing dentin.
There are two types of dentin:
- Primary dentin
- Secondary dentin.
Development time and the deposition time for both differ, primary dentin forms during tooth development, while secondary dentin forms after the tooth has erupted into the mouth. Secondary dentin is deposited at a slower rate than primary dentin and is responsible for the gradual reduction in the size of the pulp chamber.
Factors that can affect dentin growth include:
- Trauma to the tooth.
- Some antibiotics can cause discoloration of the teeth by affecting the formation of dentin.
- Top of Form
- Genetics
- Diet
Origin of dentin
Dentin is a hard, mineralized tissue that forms the bulk of the tooth structure and is located beneath the enamel and cementum. It is produced by specialized cells called odontoblasts, which are derived from the mesoderm germ layer.
Dentin is produced in two sequential phases.
- First phase: it is the synthesis and deposition of dentin (an organic matrix composed of GAGs and type I collagen)
- Second phase: It is the mineralization of dentin by hydroxyapatite to form dentin. Odontoblasts interact with enamel-forming cells at all stages of mammalian tooth formation.
Dentin formation begins at the bell stage of tooth development in the papillary tissue adjacent to the concave tip of the folded inner enamel epithelium this is the site where cuspal development begins. From this point onwards the dentin formation spreads down the cusp slope as far as the cervical loop of the enamel organ. Later the formed dentin thickens until all the coronal dentin is formed.
Similarly in multicusped teeth, dentin formation begins independently at the sites of each future cusp tip and again spreads down the cusp slopes until fusion with adjacent formative centers occurs. Dentin thus formed constitutes the dentin of the crown of the tooth or coronal dentin.
Root dentin formation requires the proliferation of epithelial cells (Hertwig’s epithelial root sheath) from the cervical loop of the enamel organ to initiate the differentiation of root odontoblasts. About two-thirds of the root dentin is formed by the time the tooth reaches its functional position.
The dental papilla is a structure that is formed in the embryonic stage of tooth development. It is located in the center of the tooth bud. As the tooth bud develops, the cells of the dental papilla differentiate into odontoblasts and begin to secrete dentin matrix.
The dentin matrix consists of collagen fibers and hydroxyapatite crystals, which are mineralized to form the hard, dense tissue of dentin. The odontoblasts continue to secrete dentin matrix throughout the life of the tooth, resulting in the continuous growth of dentin.
Thus the origin of dentin can be traced back to the mesenchymal cells of the dental papilla, which differentiate into odontoblasts and secrete the matrix that forms the hard, mineralized tissue of dentin.
Dentinogenesis: How is dentin formed?
Dentinogenesis is performed by odontoblasts, which are a special type of biological cells present on the outer layer of pulp. Dentinogenesis is the formation of dentin, a substance that forms the bulk of teeth. It begins at the late bell stage of tooth development.
Based on the different stages of dentin formation the dentin can be divided into
- Mantle dentin
- Primary dentin
- Secondary dentin
- Tertiary dentin.
Odontoblasts, which are the dentin-forming cells differentiate from cells of the dental papilla. odontoblast secrete an organic matrix around the area directly adjacent to the inner enamel epithelium which marks the future cusp of a tooth. The organic matrix contains collagen fibers with large diameters (0.1-0.2 μm in diameter).
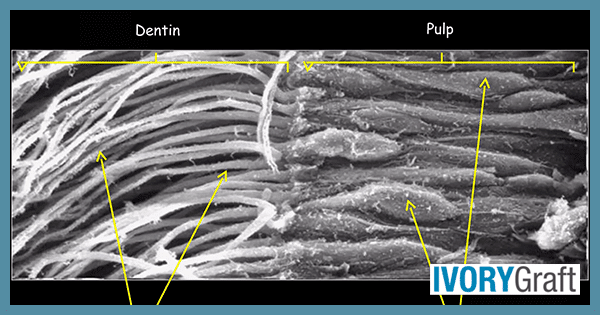
The dentin formation proceeds toward the inside of the tooth, odontoblasts begin to move toward the center of the tooth, forming an extension called the odontoblast process. These odontoblast processes secrete hydroxyapatite crystals and help in the mineralization of the matrix. This area of mineralization formed is known as mantle dentin and is a layer usually about 5-30 μm thick. Thus, mantle dentin is formed from the preexisting ground substance of the dental papilla.
However, for the formation of primary dentin, the odontoblasts increase in size, eliminating the availability of any extracellular resources to contribute to an organic matrix for mineralization. The structure of primary dentin is more tightly arranged due to the presence of larger odontoblasts which secrete collagen in smaller amounts which then undergo mineralization. Other materials (such as lipids, phosphoproteins, and phospholipids) are also secreted.
Secondary dentin is formed after root formation is finished and occurs at a much slower rate. This development continues throughout life and results in the shrinkage of pulp chambers in older age. It is not formed at a uniform rate along the tooth.
Tertiary dentin, also known as reparative dentin, forms in reaction to stimuli, such as attrition or dental caries.
In the root, the dentin is formed after Hertwig’s epithelial root sheath (HERS) appears, near the cervical loop of the enamel organ. Root dentin is different from the coronal in terms of the different orientations of collagen fibers, less amount of phosphorylation levels, and less amount of mineralization.
Which cells form dentin?
Odontoblasts are specialized ciliated cells which form the dentin. Odontoblasts synthesize dentin matrix collagens (I, type I trimer, III, V, VI) and non-collagen proteins. Odontoblasts differentiate from ecto-mesenchymal cells of the dental papilla and then progress through distinguishable stages. During odontoblast differentiation, the short, columnar-shaped pre-odontoblasts elongate and extend cellular processes toward the basement membrane where dental epithelium and ectomesenchyme interface. Fully differentiated polarized columnar are cells the secretory odontoblasts which contain numerous organelles in their supranuclear area.
Once the primary dentin is formed, the production of the secondary dentin is slowed down and persists throughout the lifetime of the tooth and secretory odontoblasts undergo some changes resulting in less polarized smaller sized cells with reduced organelles and autophagic vacuoles these are called transitional odontoblasts.
Because odontoblasts are responsible for dentinogenesis, both during tooth development and aging, the odontoblast is the most characteristic and specialized cell of the dentin-pulp complex. During dentinogenesis, the odontoblasts form dentin and the dentinal tubules, and their presence within the tubules makes dentin a living responsive tissue.
Can dentin grow back?
Dentin is considered a vital hard tissue that can grow throughout the lifetime, but it has limited ability to regenerate and can grow back to a certain extent under certain circumstances where an appropriate stimulus is given.
Examples of such cases may include:
- Tooth decay or damage: in response to tooth loss due to decay a layer of reparative dentin is deposited over the affected area. This type of dentin is tertiary dentin.
- Post pulp capping: during pulp capping, some materials such as calcium hydroxide are placed over the area where dentin is lost or present in a very less amount. Such restorative material can stimulate the formation of reparative dentin.
However, it is important to note that dentin cannot grow back completely once it has been lost due to extensive decay or trauma. In these cases, a dentist may need to use restorative materials such as fillings, crowns, or implants to replace the lost tooth structure.
Can dentin regrow enamel?
Dentin is the layer of the tooth that lies beneath the enamel and is softer and more porous than enamel. It can be stimulated to regrow in certain circumstances, as discussed above, but it cannot regrow over enamel.
Enamel is a non-vital, outermost layer of a tooth and is composed of a highly mineralized matrix of hydroxyapatite crystals. It is the hardest tissue in the human body and is not capable of regenerating itself. Once enamel is lost due to decay or erosion, it cannot be regenerated naturally by the body.
However, the lost portion of enamel can be restored by the dentist with some restorative materials which can have physical and mechanical properties like enamel.
Can you rebuild dentin?
Dentin can be stimulated to regrow to a certain extent, but once it is lost due to decay or damage, it cannot be fully rebuilt naturally. However, there are restorative treatments available to repair or replace lost dentin and restore the function and appearance of the tooth.
Some restorative treatments for dentin include:
Fillings: If the dentin has been lost due to decay, a dentist can remove the decayed portion of the tooth and place a filling made of composite resin or amalgam to restore the missing dentin.
Crowns: If a large portion of the tooth has been lost, a dentist may place a crown, which is a cap that covers the entire tooth to restore its shape, function, and appearance.
Root Canal Therapy: If the dentin has been damaged due to infection or injury, a dentist may perform root canal therapy to remove the damaged or infected pulp and place a filling material to restore the lost dentin.
Dentin Bonding: Dentin bonding is a procedure in which a dentist applies a resin material to the surface of the tooth to bond with the exposed dentin and protect it from further damage.
Overall, while dentin cannot be fully rebuilt naturally, restorative treatments are available to repair or replace lost dentin and restore the health and function of the tooth.
Can dentin regenerate?
Dentin is considered a vital hard tissue that can grow throughout the lifetime, but it has limited ability to regenerate and can grow back to a certain extent under certain circumstances where an appropriate stimulus is given.
Dentin can be stimulated to regrow to a certain extent through a process called tertiary dentinogenesis, which is a natural response of the tooth to protect itself against further damage. Tertiary dentin is a type of reparative dentin that is deposited in response to injury or damage to the pulp of the tooth. But it is important to note that dentin cannot regenerate completely once it has been lost due to extensive decay or trauma.
Pulp capping is a procedure that can stimulate dentin regeneration. During pulp capping, certain materials such as calcium hydroxide are placed on the exposed pulp of a tooth to stimulate the formation of reparative dentin. The use of stem cells and growth factors to regenerate the damaged pulp and the formation of new dentin is another area of research that has proved to be successful in dentin regeneration.
Can dentin remineralize?
Tooth enamel is a non-vital structure that is incapable of self-repairing whereas dentin and cementum have limited capacity to regenerate. With the advent of the modern tissue engineering concept and the discovery of dental stem cells, the regeneration of pulp and dentin has been tested.
Studies have shown that isolated pulp cells can be induced to differentiate into odontoblast-like cells and generate dentin-like mineral structures in vitro. In a few studies, the in vivo evidence of pulp cells capable of generating dentin has been demonstrated which proves that human pulp/dentin complex can be formed.
Dentin bridge
When the pulp is exposed due to decay or trauma, it can become inflamed and infected, which can lead to the formation of a cavity or a tooth abscess. In response to the injury, the pulp may attempt to protect itself by depositing layers of reparative dentin around the damaged area. This reparative dentin which is in response to injury or damage to the pulp of a tooth is called a dentinal bridge.
The dentinal bridge is a structure composed of multiple layers of dentin that bridges the gap between the damaged pulp and the tooth’s outer surface. A dentinal bridge is a natural response of the tooth to protect itself against injury or damage to the pulp. The dentinal bridge can help to protect the pulp from further damage and can provide a barrier against bacteria and other irritants that could cause infection.
However, if the damage is severe to the pulp, the dentinal bridge may not be enough to prevent the development of a tooth abscess or other complications. In some cases, a dentist may need to perform a root canal or other treatment to remove the damaged pulp and prevent further damage to the tooth.
Dentin enamel junction
Enamel is the hard and brittle outer portion of the tooth that cuts and grinds food and dentin is composed of a tougher biological composite, that can absorb and distribute stresses. These two major calcified tissues, enamel, and dentin, are joined by an interface known as the dentin–enamel junction (DEJ).
The DEJ is a complex and critical structure that can prevent the propagation of cracks from enamel into the dentin. The DEJ has a three-level structure, 25–100 μm scallops with their convexities directed toward the dentin and concavities toward the enamel; 2–5 μm micro scallops; and a smaller scale structure.
It is suspected that the DEJ structure plays a key role in preventing the transmission of cracks through the brittle enamel and into the tougher dentin.
Dentin regeneration
The potential of pulp tissue to self-regenerate lost dentin is well known thus regeneration of dentin relies on having vital pulps. With the advent of the modern tissue engineering concept and the discovery of dental stem cells, the regeneration of pulp and dentin has been tested.
When pulp tissue is exposed due to the loss of the overlaying dentin then a new layer of dentin is formed which is termed dentin bridge in the presence of appropriate stimuli such as using various cement-based materials for pulp cappings like calcium hydroxide and mineral trioxide aggregate (MTA).
The modes of dentin regeneration can be explained as follows:
Non-cell-based pulp/dentin tissue regeneration cell-based approach is preferable for a sizable tissue defect because the utilization of cells, especially ex vivo expanded, as a therapeutic mode is much more complex. The application of recombinant growth factors to the injured site to enhance the regeneration of dentin has been investigated for this technique.
- Stem cell-based pulp/dentin tissue regeneration
Cell-based therapy is effective for repairing extensive size defects. Stem cell-based approach provides even better results due to their potency in dividing and differentiating in response to microenvironmental cues.
DPSCs, SHED, and SCAP are the most suitable cell types used because they are derived from pulp tissue (source of DPSCs and SHED), or the precursor of pulp (source of SCAP). DPSCs and SCAP can form pieces of pulp/dentin complex.
- De novo regeneration of dental pulp and dentin
For this technique, research has been carried out in which a heterogeneous population of SCAP or DPSCs is packed into the canal space where they can serve as a scaffold. Three-four months later, the emptied canal space was found with a good quality of vascularized pulp-like tissue and more importantly, a uniform thickness of a newly generated dentin-like layer which was deposited onto the canal dentin wall as well as onto the MTA cement which was used to close the canal end.
Dentin remineralization
Dentin remineralization is a natural process that occurs in response to minor damage or decay to the tooth, during remineralization minerals, such as calcium and phosphate, are deposited back into the dentin to strengthen and repair it. This process can be enhanced through good oral hygiene practices and the use of certain dental products.
There are also several dental products available that can help to enhance dentin remineralization. For example, some toothpaste and mouthwashes contain fluoride or other remineralizing agents that can help to strengthen the teeth and prevent decay. Some dental treatments, such as fluoride varnishes or gels, can also be applied by a dentist to help promote remineralization and prevent tooth decay.
maintaining good oral hygiene practices, such as brushing twice a day with fluoride toothpaste and flossing daily is one of the best ways to promote dentin remineralization. Fluoride is a mineral that has been shown to strengthen tooth enamel and promote the remineralization of dentin. In addition, eating a healthy diet that is rich in calcium and other minerals can help to support tooth health and promote remineralization.
Dentin remineralization is a natural process that can be enhanced through good oral hygiene practices and the use of certain dental products. By taking steps to support dentin remineralization, you can help to promote overall tooth health and prevent tooth decay and other dental problems.
Dentin radiolucent
Dentin does not allow X-rays to pass through easily which means it is not normally radiolucent. However, there are certain situations in which dentin can appear radiolucent on an X-ray image.
Sclerotic dentin can appear radiolucent. Dentin sclerosis is a natural process that occurs, and it is more commonly seen in older adults. As we age, the dentinal tubules undergo calcification which makes them appear radiolucent on an X-ray.
When tooth decay penetrates through the enamel and reaches the dentin, it can cause demineralization and destruction of the dentin in this situation dentin appear radiolucent on an X-ray. Thus dental caries can lead to the formation of a cavity, which can appear radiolucent on an X-ray image.
Dentin and dental implants: osseointegration
When a dental implant is placed in the jawbone, it must form a strong bond with the bone tissue to provide a stable foundation for a dental restoration such as a crown or bridge. Osseointegration, which is the integration of a dental implant with the surrounding bone tissue is a very critical step for the success of the dental implant.
Studies have shown that dentin particles can stimulate bone growth and enhance the process of osseointegration. When dentin particles are introduced into the area surrounding the dental implant, they can promote the formation of new bone tissue and help to create a stronger bond between the implant and the surrounding bone. This is why dentin plays an important role in the process of osseointegration.
When dental implants are placed, they can create stress on the surrounding bone tissue, which can lead to bone loss over time. By placing dentin particles around the implant, this stress can be distributed more evenly, and the risk of bone loss can be reduced. Thus dentin can also help to protect the underlying bone tissue from damage caused by dental implants.
Thus, dentin can play an important role in the process of osseointegration by promoting the formation of new bone tissue and protecting the surrounding bone both of which are needed for the long-term success of dental implant treatment.
Dentin and aging: changes in tooth structure
As age advances dentin undergoes several structural changes which include the formation of dead tracts, sclerotic dentin, or reparative dentin.
Dead tracts: Odontoblast degeneration is often observed in the area of narrow pulpal horns because of the crowding of odontoblasts. Reparative dentin seals dentinal tubules at their pulpal ends, such groups of tubules may entrap air and appear black in transmitted and white in reflected light in ground sections. Dentin areas which are characterized by degenerated odontoblast processes give rise to dead tracts. Dead tracts are probably the initial step in the formation of sclerotic dentin.
Sclerotic or transparent dentin: Apatite crystals are initially only sporadic in a dentinal tubule but gradually the tubule becomes filled with a fire meshwork of crystals whenever sufficient stimuli are generated. In cases of caries, attrition, abrasion, erosion, or cavity preparation the stimuli generated are enough to cause collagen fibers and apatite crystals to begin appearing in the dentinal tubules. This condition is prevalent in older individuals. Due to the deposition of crystals, the tubule lumen is obliterated with mineral, which appears very much like the peritubular dentin. The reflective indices of dentin in which the tubules are occluded are equalized, and such areas become transparent. The crystals present in sclerotic dentin are smaller than those present in normal dentin. It is harder than normal dentin, but its fracture toughness is less, and its elastic properties are the same as normal dentin. Transparent or sclerotic dentin can be observed in the teeth of elderly people, especially in the roots, it may also be found under slowly progressing caries.
Dentin research advancements and breakthroughs
Dentin is a hard, dense, mineralized tissue that forms the bulk of a tooth. It lies beneath the enamel and cementum, and surrounds the pulp cavity. Dentin is a vital component of the tooth and plays an important role in maintaining the structural integrity and functionality of the tooth.
Recent advancements and breakthroughs in dentin research include:
Dentin regeneration: Researchers have developed new techniques for regenerating dentin, which could be used to treat dental decay and damage. These techniques involve the use of stem cells or growth factors to stimulate the formation of new dentin.
Dentin hypersensitivity: Dentin hypersensitivity, or tooth sensitivity, is a common dental problem that causes pain or discomfort in response to hot, cold, or sweet stimuli. Researchers are developing new treatments for dentin hypersensitivity, including the use of desensitizing agents and biomimetic materials that mimic the properties of natural dentin.
Dentin bonding: Dentin bonding is a technique used in restorative dentistry to attach dental materials to the tooth surface. Recent advancements in dentin bonding technology have improved the durability and longevity of restorations, reducing the need for frequent replacements.
Dentin microstructure: Researchers are studying the microstructure of dentin to better understand its mechanical properties and to develop new materials and techniques for dental restorations. By understanding the structure of dentin at a microscopic level, researchers can design more effective restorative materials and techniques.
Dentin hypersensitivity diagnosis: Recent advancements in dentin hypersensitivity diagnosis have improved our ability to identify and treat the condition. These include the use of diagnostic tools such as lasers and ultrasound, which can help to pinpoint the source of tooth sensitivity and guide treatment decisions.
Overall, these advancements and breakthroughs in dentin research have the potential to improve the diagnosis and treatment of dental conditions, leading to better oral health outcomes for patients.