This is one in a series of articles that provide detailed and updated information about Dentin.
In this specific article, which focuses on Dentin – Decay and Prevention, you can read about:
For additional articles about Dentin, see the Topic Menu.
Dentin Decay
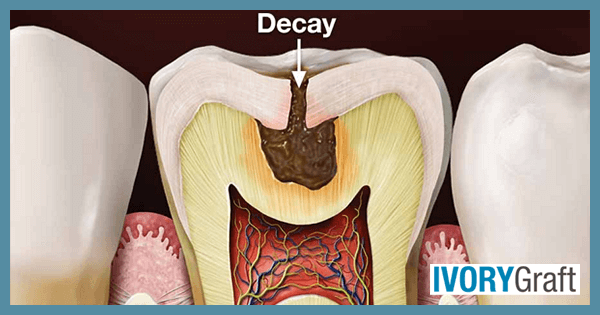
Dentin decay, also known as dental caries or cavities, occurs when the dentin layer of the tooth becomes compromised by the demineralization process, which is caused by bacteria-produced acids. The primary cause of dentin decay is the buildup of dental plaque, a sticky film composed of bacteria, food particles, and saliva. Bacteria in the plaque metabolize sugars and carbohydrates, producing acids that erode tooth enamel and dentin. Over time, this acid attack leads to the formation of cavities, which can result in tooth sensitivity, pain, and even tooth loss if left untreated.
Dentin is a hard, vital tissue located between the enamel and pulp of a tooth. Being softer than enamel, dentin is more susceptible to damage from acid, causing tooth decay to progress more rapidly once it reaches the dentin. Since dentin contains tubules that lead to the nerves of the tooth, patients may experience sensitivity when dentin is affected by tooth decay.
The signs and symptoms of dentin decay may vary depending on its extent and location:
- Discoloration (brown, black, or white) on any surface of a tooth
- Visible holes or pits in the teeth
- Tooth sensitivity
- Pain when biting down
- Mild to sharp pain when consuming sweet, hot, or cold foods and beverages
- Toothache or spontaneous pain without any apparent cause
In the case of existing dentin decay, your dentist may recommend treatments such as dental fillings, crowns, or root canal therapy, depending on the severity of the decay. Early detection and intervention are crucial for preserving the tooth structure and preventing more invasive treatments.
Can you stop dentin decay?
Although dentin decay cannot be reversed, it can be stopped. After a clinical examination by a dentist to determine the site and extent of decay, several procedures can be performed to halt and treat it. The decayed tooth undergoes cavity preparation, during which all affected dentin is removed. A restorative material is then placed to seal the cavity.
The type of filling or restoration depends on the depth of decay. If the decay is not too deep, a routine restoration is sufficient. However, for extensive and deep decay, a layer of calcium hydroxide is placed prior to restoration to promote secondary dentin formation.
The most effective way to prevent dentin decay is to practice good oral hygiene habits, such as brushing your teeth twice a day with fluoride toothpaste, flossing daily, and using an antiseptic mouthwash. Additionally, avoid sugary and acidic foods and beverages, as these can contribute to the development of decay.
Can you brush dentin away?
The outermost layer present in the tooth is enamel. Due to improper brushing techniques or with the usage of hard bristles toothbrushes the enamel may get abraded and as a result, expose the underlying dentin.
The surface of dentin is more porous than the enamel which over a period of time may get lost further.
If an aggressive and improper brushing technique is followed for a longer period of time then not only the enamel but the gums may also get affected and as a result, the dentin in the root portion may also get exposed. Which can later follow the same wearing-off process as the coronal dentin.
How can I Fix dentin decay Naturally?
Dentin is the hard tissue located between the enamel and pulp of a tooth. Once it is lost, it cannot regenerate. Although there are natural remedies that may help relieve symptoms associated with dentin hypersensitivity, If there is any dentin decay or damage – the only way to restore dentin is through proper dental procedures.
Natural remedies for dentin hypersensitivity relief include:
- Green Tea: Drinking green tea, which contains antioxidants and anti-inflammatory compounds, may help reduce inflammation and relieve pain associated with dentin hypersensitivity.
- Warm Saltwater Rinse: Rinsing your mouth with warm salt water can help reduce inflammation and relieve pain associated with dentin hypersensitivity.
- Guava Leaves: Chewing guava leaves or using a topical gel containing guava leaf extract may help reduce tooth pain and sensitivity.
- Garlic: Garlic contains allicin, a natural antibacterial and anti-inflammatory agent. Chewing on a piece of garlic may help reduce pain and inflammation associated with dentin hypersensitivity.
- Clove Oil: Applying clove oil to the affected tooth may help reduce pain and inflammation. Clove oil contains a natural anesthetic called eugenol, which can help numb the area and reduce pain.
- Capsaicin: Capsaicin, a spicy substance found in chili peppers, can cause a burning sensation when applied to the skin or gums. However, it may also help reduce pain associated with dentin hypersensitivity.
- Turmeric: Turmeric, a yellow spice used in Ayurvedic medicine, contains curcumin, which may help relieve pain due to its anti-inflammatory properties.
While these natural remedies may provide temporary relief from the symptoms of dentin hypersensitivity, they cannot repair dentin. If you have dentin decay or damage, it is crucial to seek proper dental treatment.
Can toothpaste repair dentin?
Once the decay has progressed past the enamel and into the dentin, toothpaste cannot repair the damage. However, some toothpaste brands which contain fluoride can help prevent further damage to the dentin and even repair some of the early signs of tooth decay.
Fluorides are traditionally used as a caries preventive material which can help in the remineralization of enamel/dentin. In addition to this, there are various clinical trials that have shown that application of fluoride solution can also decrease dentinal hypersensitivity.
SEM revealed granular precipitates that appear in the peritubular dentin after the application of fluorides. These precipitates are of calcium fluoride crystals which can decrease the dentinal permeability by precipitation inside the dentinal tubules. These crystals are partially insoluble in saliva.
Fluoride works by strengthening the tooth enamel, which is the hard outer layer of the tooth. When the enamel is strong, it is more resistant to acid attacks from bacteria in the mouth, which can help prevent tooth decay from progressing and reaching the dentin.
Can Dentin Decay Be Reversed?
Dentin is a hard tissue located between the enamel and pulp of a tooth, and it is less dense than enamel. The extent of dentin decay varies depending on the size and depth of the lesion, which determines whether it can be reversed.
If there is only minor demineralization or surface dentin loss due to the acidic environment created by bacteria, the decay process can be reversed. Maintaining good oral hygiene, avoiding hard and sugary foods, using fluoridated toothpaste, and undergoing complete oral prophylaxis with a dental professional can help with this reversal.
However, when decay reaches the inner layer of dentin, it cannot be reversed. In such cases, the decay can be stopped or corrected through complete decay removal and tooth restoration with a suitable restorative material.
Dentin Erosion
Dentin erosion refers to the loss of dentin substance due to chemical processes, and not involving bacteria (in contrast to dentin decay).
Dentin erosion is caused by chemical processes involving various intrinsic and extrinsic factors, including:
- Intrinsic factors include endogenous acids, such as gastric acids that contact teeth in patients with anorexia, bulimia, gastroesophageal reflux disease (GERD),or other gastrointestinal disturbances.
- Extrinsic factors relate to the frequent consumption of acidic foods or beverages and exposure to acidic contaminants. Industrialized beverages, especially soft drinks, and citric fruits and juices can significantly increase the prevalence of dental erosion.
Some common signs and symptoms associated with dentin erosion include:
- Tooth sensitivity: As the dentin erodes, it exposes the underlying nerves, leading to increased sensitivity to hot, cold, or sweet stimuli.
- Discoloration: Eroded dentin may appear discolored or yellow, as the enamel becomes thinner and exposes the underlying dentin.
- Changes in tooth shape: The erosion of dentin may cause teeth to lose their original shape or become rounded.
- Translucency: The edges of front teeth may appear translucent due to enamel thinning.
- Cracks or chips: Eroded teeth may become more susceptible to cracks or chips.
Dental erosion is more common among young people, primarily due to lifestyle changes. There has been a 50% increase in soft drink consumption over the past few decades, particularly among children and adolescents. These dietary changes, combined with inadequate oral hygiene, have contributed to the rise in dental erosion cases.
The development of erosion involves a chemical process that demineralizes the tooth’s inorganic phase, reducing the hardness of the tooth substrates. Abrasive challenges from brushing further increase the loss of tooth substrates. The loss of substance due to erosion is a dynamic process with periods of demineralization and remineralization.
Dentin and Dental Abrasion
Dental abrasion refers to the loss of tooth structure caused by mechanical forces from a foreign element, as opposed to dental attrition (caused by tooth-to-tooth contact during normal physiological activities, such as chewing and grinding).
Some common causes of dental abrasion include:
- Aggressive tooth brushing: Using a hard-bristled toothbrush or applying excessive pressure while brushing can cause the enamel and dentin to wear away, especially near the gum line.
- Foreign objects: The habit of using toothpicks, pins, or other sharp objects to remove food particles from between teeth can lead to dental abrasion.
- Abrasive toothpaste: Some toothpastes contain abrasive particles that may contribute to tooth wear if used excessively or with improper brushing techniques.
- Oral appliances: Ill-fitting dentures, braces, or other oral appliances can cause friction against the tooth surface, leading to abrasion.
When the mechanical force starts at the cementoenamel junction, tooth loss can progress rapidly because the enamel is thin in this region. Once the enamel is worn away, the softer dentin and cementum structures are quickly damaged by abrasion.
The condition often appears as a V-shaped notch, usually caused by excessive pressure during tooth brushing. Premolars and canines are the teeth most commonly affected. Abraded areas typically display worn, shiny surfaces, often with a yellow or brown tinge near the cervical margin.
If you suspect dental abrasion or experience any related symptoms, consult a dental professional for an evaluation and appropriate treatment to preserve your oral health and prevent further damage.
Dentin Sealer and Immediate Dentin Sealing (IDS)
A dentin sealer, also known as a dental bonding agent, is a material used by dentists to protect and seal the dentin layer of a tooth, especially when it has been exposed during tooth preparation for indirect restorations such as inlays, onlays, or crowns. The primary purpose of a dentin sealer is to create a protective barrier between the dentin and the restorative material, preventing sensitivity, discomfort, and potential damage to the pulp. Protecting the dental pulp is a top priority for dentists, as it improves clinical outcomes and prevents patient sensitivity and pain.
The process of dentin sealing involves several steps:
- Tooth preparation: The dentist removes the decayed or damaged tooth structure and prepares the tooth for indirect restoration.
- Application of dentin sealer: The dentist applies a bonding agent to the freshly cut dentin, following the manufacturer’s instructions for the chosen product.
- Light curing: The bonding agent is typically light-cured using a dental curing light to ensure proper polymerization and adhesion to the tooth surface.
- Placement of restoration: Once the dentin sealer has been applied and cured, the dentist can proceed with the placement of the final restoration, such as an inlay, onlay, or crown.
Immediate dentin sealing (IDS) is a procedure that involves applying a dentin bonding agent to freshly cut dentin when it is exposed during tooth preparation for indirect restorations. IDS is an advanced protocol designed for the temporization and final cementation of indirect restorative procedures, offering several distinct advantages.
In conventional procedures, dentin sealing is delayed and the sealing of dentin tubules takes place during the bonding stage of the final restoration. A clean dentin surface is essential for optimal sealing and adhesion. The goal of IDS is to create a hybrid layer that both mimics the dentin-enamel junction (DEJ) and promotes proper adaptation and adherence to the final restoration, which aligns with the principles of minimal intervention dentistry.
It is essential to consult with a dental professional for appropriate treatment options and to ensure the proper application of dentin sealers for the best clinical outcomes.
Dentin Sialo-Phosphoprotein
Dentin Dentin Sialo-Phosphoprotein (DSPP) is a protein found in dentin that is essential for the normal mineralization (hardening) of teeth. During tooth development, DSPP is broken down into three proteins: dentin sialoprotein (DSP), dentin glycoprotein (DGP), and dentin phosphoprotein (DPP). These proteins work together to regulate the formation of hydroxyapatite crystals, the primary mineral component of dentin.
The DSPP gene, which codes for the dentin Sialo-Phosphoprotein, is located on chromosome 4 in humans. Mutations in this gene can lead to various dental disorders, such as dentinogenesis imperfecta-1. Dentinogenesis imperfecta is a hereditary condition characterized by weak, discolored, and brittle teeth due to abnormal dentin formation. In some individuals, dentinogenesis imperfecta occurs in combination with an autosomal dominant form of deafness. Allelic differences due to repeat polymorphisms have been found for this gene.
The study of DSPP and its related proteins has improved our understanding of tooth development and the molecular mechanisms underlying dentin formation. This knowledge has potential applications in dental treatments, such as the development of novel biomaterials for tooth repair or the design of gene therapies for dental disorders caused by DSPP mutations. Additionally, research on Dentin Sialo-Phosphoprotein may contribute to a broader understanding of biomineralization processes in other tissues and organisms.
Dentin Varnish
Varnishes are coating materials that are applied to surfaces in a thin layer, forming a continuous and solid film after undergoing chemical or physical changes. Depending on their intended use or necessary processing conditions, varnishes are employed in liquid or powder form. A good varnish should be comfortable for the patient, easy and safe to apply, have good storage stability, and be homogeneous.
Types of Dental Varnishes include:
- Fluoride varnish: This type of varnish provides protection from demineralization and erosion. Examples include Duraphat (2.2% fluoride), Carex (1.8% fluoride), and Fluoroprotector (0.7% fluoride).
- Antimicrobial varnish: Antimicrobial protective varnishes can reduce bacteria and help shift the bacterial balance to a normal level. Chlorhexidine thymol varnish is a commonly used antimicrobial varnish that has antimicrobial activity against both gram-positive and gram-negative microorganisms.
- Desensitizing varnish: Mainly used for dentinal sensitivity purposes, desensitizing varnishes are contraindicated in ulcerative gingivitis and stomatitis.
- Tooth whitening varnish: These varnishes contain peroxides that diffuse into the tooth after application. The decomposition of these oxides produces oxygen, which converts stains and discoloration into colorless compounds, making them useful for tooth whitening purposes.
Dental varnishes can be classified based on their curing activity, which refers to the process of setting or hardening once applied to the teeth. There are two main types of dental varnishes based on curing activity: physically cured varnishes and chemically cured varnishes:
- Physically cured varnishes: These varnishes harden through physical processes such as evaporation of solvents or cooling. Once applied to the tooth surface, the solvent in the varnish evaporates or cools, causing the varnish to set and form a solid film. This type of varnish is typically easy to apply and does not require any special equipment or additional chemicals to initiate the curing process. However, the drying time may be longer, and the final hardness might be less compared to chemically cured varnishes.
- Chemically cured varnishes: In contrast to physically cured varnishes, chemically cured varnishes rely on a chemical reaction to initiate the curing process. These varnishes often consist of two components: a base and a catalyst. When mixed together, the base and catalyst undergo a chemical reaction that causes the varnish to set and harden. Chemically cured varnishes usually provide a more durable and long-lasting protective layer compared to physically cured varnishes. However, they might require more precise handling during application, as the curing process starts immediately after mixing the components.
Both types of dental varnishes offer different advantages and disadvantages, and the choice between them depends on factors such as the specific dental application, the desired level of protection, and the practitioner’s preference.
Pulp-Dentin Complex and Dental Pulp Protection
The dental pulp is a unique, soft tissue of mesenchymal origin containing specialized cells known as odontoblasts. These cells are arranged peripherally, in direct contact with the dentin matrix that surrounds the entire tooth root and is covered by a thin layer of cement. In the crown, beneath the enamel layer, the main internal part of the tooth is referred to as the “dentin-pulp complex“.
The dentin-pulp complex is characterized by the close relationship between odontoblasts and dentin. Dentin, a highly mineralized tooth tissue, encloses the pulp chamber and root canals, maintaining their structural integrity and isolation. Therefore, dentin and pulp should be considered a functional entity comprised of histologically distinct constituents.
This complex responds dynamically as a functional unit to various stimuli, such as caries, trauma, chemical agents, or other aggressors. It protects the pulp tissue through the formation of sclerotic dentin, calcification of dentin tubules, or by promoting reparative dentin formation by the pulpal odontoblasts. Pulp cells and odontoblasts play a critical role in regenerating damaged dentin, serving as a protective physical defense against exogenous stimuli by depositing tertiary dentin on the pulp chamber surface.
When dentin is invaded by pathogens and their byproducts, the first pulp cells to respond are the odontoblasts. These cells, situated at the dentin-pulp complex, have a long cellular process embedded in dentin tubules, representing the first line of defense.
Three basic reactions protect the pulp from injury occur simultaneously, with their rate varying depending on the strength of the stimuli and the aggressive nature of the advancing lesion:
- Inflammatory and immune reactions: The dental pulp contains immune cells, which mount an inflammatory response to fight off infections or mitigate damage from other harmful stimuli. The immune response helps to clear out pathogens and promote tissue repair.
- Tertiary dentin formation: In response to injury or external stimuli, odontoblasts produce tertiary dentin, a reparative dentin layer that acts as a barrier to protect the pulp. This new layer of dentin can either be reactionary, formed by existing odontoblasts, or reparative, formed by newly differentiated odontoblast-like cells when the original odontoblasts are damaged.
- Decreased dentin permeability: The dentin’s permeability can be reduced by the formation of sclerotic dentin or the calcification of dentin tubules. These changes limit the movement of fluids and harmful substances through the dentin, providing an additional layer of protection for the dental pulp.
Maintaining the health of the pulp-dentin complex is essential for the longevity and vitality of a tooth. Dental professionals must carefully consider the potential impact of dental treatments on this complex to ensure that pulp protection is maintained and the risk of complications, such as pulpitis or pulp necrosis, is minimized.
Dentin Sealing Agents and Desensitizers
Dentin sealing agents and desensitizers are products designed to alleviate tooth sensitivity caused by exposed dentin. Dentin, the layer of the tooth beneath the enamel, contains tiny tubules leading to the tooth’s nerves. When enamel wears away or gums recede, dentin becomes exposed, and the tubules can cause tooth sensitivity.
Dentin sealing agents create a barrier over the exposed dentin to protect the tubules from external stimuli. They typically contain ingredients such as resin, fluoride, or calcium phosphate, which bond to the tooth surface and seal the tubules. Examples of dentin sealing agents include resin-based materials like bonding agents or sealants, glass ionomer cement, and calcium phosphate-based materials.
Desensitizers, in contrast, work by blocking the nerve impulses responsible for tooth sensitivity. They typically contain ingredients such as potassium nitrate, strontium chloride, or fluoride, which penetrate the tubules and help desensitize the nerves. Examples of desensitizers include toothpaste or gels for sensitive teeth, fluoride varnishes, and in-office treatments like laser therapy or dental bonding.
It is important to note that while dentin sealing agents and desensitizers can effectively reduce tooth sensitivity, they may not be suitable for all cases. It is essential to consult a dentist to determine the best course of treatment for your individual needs.
Dentin and Oral Hygiene Practices
Dentin is a layer of the tooth located beneath the enamel, containing tiny tubules leading to the tooth’s nerves. As dentin is less hard and more porous than enamel, acidic byproducts from bacteria can cause decay in the dentin. Good oral hygiene practices and a proper diet can help prevent dentin exposure and maintain dental health.
Some oral hygiene practices that contribute to healthy dentin include:
- Low sugar and acids: Limiting the consumption of sugary and acidic foods and drinks, as they can erode tooth enamel and expose dentin, leading to tooth sensitivity.
- Proper brushing: teeth twice a day for two minutes each time using fluoridated toothpaste, which helps remove plaque and bacteria that can cause tooth decay and gum disease. Proper brushing techniques should be followed.
- Antiseptic mouthwash: Using an antiseptic mouthwash to kill bacteria in the mouth and freshen breath.
- Flossing: Routine flossing to remove food particles and plaque from between teeth and along the gum line, where a toothbrush cannot reach. This practice can also help maintain bone levels by preventing interdental bone loss.
- Dental Checkups: Scheduling regular dental checkups, which can help catch dental issues early and prevent them from progressing into more severe problems. It is generally advised to visit the dentist every six months for a routine checkup.
- Desensitizing Products: Using toothpaste or mouthwash designed for sensitive teeth in cases of sensitivity, which can help reduce discomfort and protect exposed dentin.
By following these oral hygiene practices, dentin can be protected, and tooth sensitivity can be prevented.