This is one in a series of articles that provide detailed and updated information about Dentin.
In this specific article, which focuses on Dentin – Anatomy and Histology, you can read about:
For additional articles about Dentin, see the Topic Menu.
Dentin Anatomy
Dentin is a vital, hard, mineralized tissue that forms the bulk of the tooth structure. In the crown portion, it is found between the enamel layer and the pulp, while in the roots, it is found between the cementum and the pulp. Dentin is composed of a dense organic matrix of collagen fibers and hydroxyapatite crystals, as well as small spaces called dentinal tubules that run through the tissue.
The anatomy of dentin can be explained as follows:
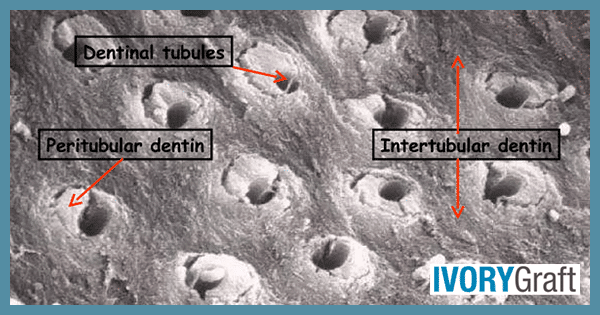
- Dentinal tubules: These microscopic structures run from the dentin-enamel junction to the dentino-pulpal junction. The tubules contain processes of specialized cells called odontoblasts, which secrete the organic components of dentin and regulate its mineralization. The dentinal tubules also contain fluid and nerve fibers that transmit sensory information from the tooth surface to the dental pulp.
- Peritubular dentin: This highly mineralized dentin surrounds the dentinal tubules, making it harder and more brittle than the surrounding intertubular dentin. It is composed of densely packed hydroxyapatite crystals.
- Intertubular dentin: This type of dentin makes up the bulk of the tissue and is less mineralized than peritubular dentin. It contains collagen fibers and hydroxyapatite crystals, making it more elastic and flexible than peritubular dentin and providing the tissue with its overall toughness and resilience.
- Mantle dentin: As the outermost layer of dentin, it is found immediately next to the enamel. Mantle dentin has a higher mineral content and smaller dentinal tubules that are oriented perpendicular to the tooth surface compared to the underlying circumpulpal dentin.
- Circumpulpal dentin: This innermost layer of dentin is found adjacent to the dental pulp. It is less mineralized than mantle dentin and contains larger dentinal tubules that are oriented parallel to the long axis of the tooth.
Where is Dentin Found in the Tooth?
Dentin is a hard, vital tissue located in the middle layer of the tooth, situated between the outer enamel layer and the inner pulp chamber. The dentin layer is thickest in the crown of the tooth (the part visible above the gum line) and progressively thins toward the root. The thickness of the dentin layer can vary depending on the location within the tooth and the individual. Dentin contains living cells and is sensitive to various stimuli, such as temperature, pressure, and chemical agents. The sensory nerve fibers that transmit this information from the dentin to the dental pulp are located within the dentinal tubules running through the tissue.
Dentin performs various critical functions, from supporting the enamel to protecting the pulp. It forms a basis for tooth attachment to the surrounding bone and ligaments.
Types of Dentin: Primary, Secondary, and Tertiary
Dentin is a vital, hard, mineralized tissue that forms the bulk of the tooth structure. In the crown portion, it is found between the enamel layer and the pulp, while in the roots, it is found between the cementum and the pulp. Dentin is composed of a dense organic matrix of collagen fibers and hydroxyapatite crystals, as well as small spaces called dentinal tubules that run through the tissue.
There are three types of dentin, classified based on their mechanism and timing of formation:
- Primary dentin: the initial layer of dentin that is formed during tooth development.
- Secondary dentin: This is a layer of dentin produced after the root of the tooth is completely formed.
- Tertiary dentin: This type of dentin is created in response to a stimulus (carious attack, trauma, etc.)
Primary dentin: This initial layer of dentin is the most predominant type of dentin and is responsible for providing the tooth with its basic structure and support. Primary dentin can be further categorized into three types of dentin:
- Mantle Dentin: This is the outermost layer of primary dentin, found immediately next to the enamel. It is approximately 150 micrometers thick and is formed by newly differentiated odontoblasts. Mantle dentin has loosely packed collagen fibrils and is less mineralized compared to other types of dentin. It also lacks phosphorylation, a characteristic that distinguishes it from the rest of the primary dentin.
- Circumpulpal Dentin: This type of dentin is more mineralized and makes up the majority of the dentin layer. It is found beneath the Mantle dentin layer and is secreted by odontoblasts after the Mantle dentin has been formed. Circumpulpal dentin provides the tooth with its overall toughness and resilience, as well as forming the bulk of the tooth structure. Circumpulpal dentin forms before the root formation is completed.
- Predentin: This newly secreted, unmineralized dentin is typically 10-47 micrometers thick, lines the innermost region of the dentin, adjacent to the dental pulp. It consists of collagen, glycoproteins, and proteoglycans. Predentin is less mineralized than other types of dentin and stains less intensely in histological preparations, such as hematoxylin and eosin-stained sections. Over time, predentin undergoes a mineralization process, transforming into a mature dentin structure. This continuous process of predentin secretion and mineralization allows for the growth and repair of dentin throughout the life of a tooth.
Secondary dentin: This type of dentin is formed after root formation is complete, normally after the tooth has erupted and is functional. Secondary dentin has a similar structure to primary dentin, although its deposition is not always even around the pulp chamber. It grows significantly slower than primary dentin. As secondary dentin accumulates, the pulp chamber size decreases, a process known as pulp recession. This natural occurrence is associated with aging.
Tertiary dentin: This dentin is formed in response to specific stimuli or injury, such as a carious attack or trauma to the tooth. It is deposited at injured sites by odontoblasts or replacement odontoblasts from the pulp (undifferentiated mesenchymal cells). Tertiary dentin can be further classified into two categories: reactionary and reparative dentin:
- Reactionary Tertiary dentin: This type of dentin is secreted by existing odontoblasts in response to mild stimuli, such as chemical attacks or bacterial metabolites. It helps slow down the progress of dentin loss and to protect the dental pulp. For instance, during a carious attack toxic substances diffuse through the dentinal tubules, prompting odontoblasts to form reactionary tertiary dentin.
- Reparative tertiary dentin: When more severe injuries occur, such as extensive dentin loss due to infection or odontoblast death, undifferentiated mesenchymal cells can differentiate into odontoblast-like cells. These new cells secrete reparative tertiary dentin underneath the site of the attack. This process not only slows down the progression of the injury but also prevents bacteria and their metabolites from reaching the pulp, reducing the likelihood of partial pulp necrosis.
It is important to differentiate between these two types of tertiary dentin, as they are secreted in different situations and by different cells.
Both types of tertiary dentin are deposited in response to stimuli, and the rate of deposition may vary. When deposited rapidly, with a sparse and irregular tubular pattern and some cellular inclusions, it is referred to as “osteodentin.” However, if the stimulus is less active, the dentin is laid down slowly with a more regular tubular pattern and without cellular inclusions. In such cases, calcium salts may be deposited in or around degenerated odontoblastic processes and may obliterate the tubules. This type of dentin is called “transparent” or “sclerotic dentin.”
In ground sections of dentin, the disintegrated odontoblastic processes appear as empty tubules filled with air. They appear dark in transmitted light and white in reflected light. This type of dentin is called “dead tracts” and represents an area of decreased sensitivity. Reparative dentin seals these dead tracts at their pulpal end.
Mantle Dentin
Mantle dentin is the outermost layer of dentin that lies immediately adjacent to the enamel layer of the tooth. With a more organized structure and higher mineral content than the underlying dentin, mantle dentin forms a collar around the tooth crown, as its name suggests.
The specialized cells called odontoblasts, which produce dentin and are present in mantle dentin, also play a role in signaling the enamel-forming cells called ameloblasts to secrete the enamel matrix. During tooth development, enamel formation occurs in a highly regulated manner that depends on the presence and function of the underlying mantle dentin.
The collagen fibers in mantle dentin are oriented in a way that promotes the attachment of the periodontal ligament fibers, which anchor the tooth to the surrounding bone. Thus, mantle dentin plays an important role in the formation and structure of tooth enamel and is also involved in the attachment of the tooth to the surrounding bone and ligaments.
When is Secondary Dentin Formed?
Secondary dentin forms after root formation is complete, typically after the tooth has erupted and become functional. It has a structure similar to primary dentin, but its deposition is not always even around the pulp chamber. Secondary dentin grows much more slowly than primary dentin. As secondary dentin accumulates over time, the size of the pulp chamber decreases with age, a process known as pulp recession.
When is Tertiary Dentin Formed?
Tertiary dentin forms in response to various types of stimuli, such as injury or irritation to the pulp tissue that can expose the pulp chamber or damage the tooth. This type of dentin is deposited by specialized cells called odontoblasts. Tertiary dentin can be divided into reactionary and reparative dentin:
- Reactionary Tertiary Dentin: Secreted by odontoblasts in response to chemical attacks or bacterial metabolites, reactionary tertiary dentin helps slow down dentin loss and protect the pulp. For example, during a carious attack, toxins diffuse down the dentinal tubules, activating the odontoblasts to form reactionary tertiary dentin.
- Reparative Tertiary Dentin: When dentinal tissue is lost due to infection that reaches near the pulp, or in cases of odontoblast death, undifferentiated mesenchymal cells can differentiate into odontoblast-like cells. These cells then secrete reparative tertiary dentin underneath the site of the attack. This not only slows down the progression of the attack but also prevents bacteria and their metabolites from diffusing into the pulp, reducing the likelihood of partial pulp necrosis.
It is important to differentiate between these two types of tertiary dentin, as they are secreted in different situations and by different cells.
What Type of Dentin Borders the Pulp?
Peritubular dentin, also known as Circumpulpal dentin, borders the pulp. It is closest to the pulp tissue and surrounds the dentinal tubules that contain the processes of the odontoblast cells. The peritubular dentin is highly mineralized and contains a high concentration of collagen fibers that form a dense network around the tubules.
The thickness and structure of the peritubular dentin can vary depending on the location within the tooth and individual variations. In regions where the dentin is exposed to external stimuli, such as areas affected by dental caries or trauma, the peritubular dentin may be thicker and contain more irregularities in its structure.
The peritubular dentin is responsible for dentin sensitivity, as the sensory nerve fibers that transmit sensations from the dentin to the pulp tissue are located within the dentinal tubules present in the circumpulpal/peritubular dentin. This type of dentin provides protection and structural support to the pulp tissue and is also involved in the exchange of nutrients and waste products between the pulp tissue and the dentinal tubules.
Dentin Structure
The composition of dentin can be described as follows:
- Organic matrix: Accounting for almost 35% of the dentin composition, the organic matrix can be divided into collagenous and non-collagenous components. The collagenous part is primarily composed of Type I collagen, which holds the hydroxyapatite mineral crystals. Dentin has more organic content but less mineral than enamel. Small amounts of Type III and Type V collagen are also present. The non-collagenous components include phosphorylated and non-phosphorylated proteins, proteoglycans, lipids, growth factors, and enzymes.
- Mineral content: Comprising approximately 50% of the dentin composition, the mineral content is primarily composed of hydroxyapatite, which gives dentin its hardness and density. This crystalline calcium phosphate form features plate-shaped crystals, smaller than those in enamel. Additionally, dentin contains small amounts of phosphates, carbonates, sulfates, as well as collagen and other proteins. These organic materials provide flexibility and toughness to dentin, allowing it to withstand the stresses of biting and chewing.
- Water: this accounts for the remaining 15-20% of dentin composition.
Dentin consists of microscopic channels called dentinal tubules, which radiate outward through the dentin from the pulp to the exterior cementum or enamel border. The dentinal tubules extend from the dentin-enamel junction (DEJ) in the crown area or the dentinocemental junction (DCJ) in the root area to the outer wall of the pulp. These tubules contain fluid and cellular structures (Tome’s fiber).
The diameter of dentinal tubules is larger near the pulpal cavity (3-4 µm) and smaller at their outer ends (1 µm). The terminal part of the dentinal tubules branches into 2-3 branches near the DEJ, resulting in an increased number of dentinal tubules in this area. Lateral branches of dentinal tubules, called canaliculi, also exist.
The course of dentinal tubules is curved, resembling an ‘S’ shape known as primary curvature. Starting at right angles from the pulpal surface and ending perpendicular to the DEJ, this configuration indicates the course taken by odontoblasts during dentinogenesis. In the root and the area of the incisal edge or cusps, the dentinal tubules are almost straight. The tubules are farther apart in the peripheral layers and more closely packed near the pulp.
There is a 1 µm thick sheath of peritubular dentin surrounding each tubule (about 0.75 µm near the DEJ and 0.4 µm near the pulp). Peritubular dentin is highly calcified and is about 40% more calcified than adjacent intertubular dentin. Intertubular dentin, located between the dentinal tubules, forms most of the dentin. It is less mineralized than peritubular dentin and consists of a coarse network of collagen fibers in which apatite crystals are deposited.
Which Dentin is the Most Highly Mineralized?
Mantle dentin, the outermost layer of dentin closest to the enamel layer of the tooth, is the most highly mineralized dentin. It has a higher mineral content than the underlying dentin layers, making it harder and more resistant to wear and decay. Mantle dentin has a more organized structure and forms a collar around the tooth crown, as its name suggests.
Specialized cells called odontoblasts, which produce dentin and are present in mantle dentin, play a role in signaling enamel-forming cells called ameloblasts to secrete the enamel matrix. During tooth development, enamel formation occurs in a highly regulated manner that depends on the presence and function of the underlying mantle dentin. The collagen fibers in mantle dentin are oriented in a way that promotes the attachment of the periodontal ligament fibers, which anchor the tooth to the surrounding bone.
Circumpulpal Dentin
Circumpulpal dentin, also known as the inner dentin, is a mineralized dentin that makes up most of the dentin layer and is present beneath mantle dentin. It is secreted by odontoblasts after the layer of mantle dentin has formed. Circumpulpal dentin forms before the completion of root formation. Odontoblasts initially produce dentin, which undergoes mineralization and becomes mineralized dentin.
The generation of circumpulpal dentin takes place rhythmically, with daily incremental (von Ebner’s) lines appearing at each 4 μm interval. This circadian rhythm interacts with another longer-period rhythm, forming Owen’s lines, which appear every 16–20 μm. The daily production of dentin decreases from 10 μm/day at the onset of dentin formation to 4 μm/day. The continual centripetal formation of circumpulpal dentin results in the gradual reduction of pulp volume.
Circumpulpal dentin contains about 20,000 dentinal tubules per mm2, with variations between the outer and inner parts of the dentin layer. Due to space restrictions, more tubules are present in the inner third than in the outer third (between 18,000 and 21,000/mm2). The tubules are curved, displaying a gradual S-shape from the dentin-enamel junction to the pulp. The primary dentin of the crown and most of the root is formed before eruption. The curvature is more accentuated in tubules formed after the tooth erupts.
Circumpulpal dentin plays several essential roles in tooth function and health:
- Protection: It provides a protective barrier for the dental pulp, shielding it from mechanical, thermal, and chemical stimuli that could cause inflammation or damage to the pulp tissue.
- Support: Circumpulpal dentin contributes to the structural integrity of the tooth, providing support and stability to both the enamel and the cementum.
- Sensitivity: The dentinal tubules in circumpulpal dentin contain sensory nerve fibers that transmit sensations from the tooth surface to the pulp tissue, allowing the tooth to respond to external stimuli such as temperature or pressure.
- Nutrient and waste exchange: The dentinal tubules facilitate the exchange of nutrients and waste products between the dental pulp and the surrounding dentin, maintaining the health and vitality of the tooth.
Sclerotic Dentin
Sclerotic dentin is a type of dentin that forms in response to chronic irritants or stimuli, such as dental caries or aging. This dentin is characterized by the deposition of mineralized tissue within the dentinal tubules, which can be identified by its distinct appearance under a dental microscope. When a stimulus is less active, reparative dentin is laid down slowly, exhibiting a more regular tubular pattern without cellular inclusions. In such cases, calcium salts may be deposited in or around degenerated odontoblastic processes, potentially obliterating the tubules. This type of dentin is also referred to as “transparent” or “sclerotic dentin.”
The formation of sclerotic dentin serves as a natural defense mechanism for the tooth, protecting the pulp from further damage. However, excessive deposition of sclerotic dentin can also lead to reduced fluid flow and decreased tooth sensitivity.
Dentinal Tubules
Dentin contains microscopic channels called dentinal tubules, which radiate outward from the pulp to the exterior cementum or enamel border. These tubules extend from the dentin enamel junction (DEJ) in the crown area or the dentinocemental junction (DCJ) in the root area to the outer wall of the pulp. They house fluid and cellular structures called Tomes’ fibers. The diameter of dentinal tubules is larger near the pulp cavity (3-4 µm) and smaller at their outer ends (1 µm). Near the DEJ, the terminal part of the dentinal tubules branches into two or three smaller branches, resulting in an increased number of tubules in this area. Additionally, there are lateral branches called canaliculi.
The course of dentinal tubules is curved, resembling an ‘S’ shape known as primary curvature. This configuration, starting at right angles from the pulp surface and ending perpendicular to the DEJ, indicates the path taken by odontoblasts during dentinogenesis. In the root and incisal edge or cuspal areas, the dentinal tubules are almost straight. The tubules are farther apart in peripheral layers and more closely packed near the pulp.
Dentinal tubules play a crucial role in tooth formation and function, as they facilitate the exchange of nutrients and waste products between the pulp tissue and surrounding dentin. They also enable the transmission of sensory signals from the dentin to the pulp tissue.
Intratubular dentin
Intratubular dentin is found within the dentinal tubules, which are the tiny channels that run from the tooth’s outer surface to the pulp chamber in the center. These tubules contain the hard, calcified tissue that makes up the bulk of a tooth. Intratubular dentin forms when odontoblasts, the specialized cells that line the pulp chamber, deposit new mineralized tissue within the tubules. This process can occur in response to various stimuli, such as dental caries or other forms of tooth damage.
The formation of intratubular dentin is an essential mechanism by which the tooth can repair itself and protect the pulp from further damage. However, excessive deposition of intratubular dentin can also cause problems, such as narrowing of the tubules and reduced fluid flow, which can affect the tooth’s sensitivity.
What are Dentin Islands?
Dentin islands, first described by French anatomist Eugene Nasse in the early 19th century, are small, oval-shaped clusters of cells found in the dental pulp of teeth. They are also known as “Islands of odontoblasts” or “Islets of Nasse.” Surrounded by dentin, they are composed of odontoblasts, specialized cells responsible for the formation of dentin.
Dentin islands are thought to contribute to the repair process by laying down new dentin in response to damage. As such, they are believed to play a role in the formation of tertiary dentin, a type of dentin that forms in response to injury or irritation to the tooth.
Dentin Histology
Dentin is a calcified tissue of the body, typically covered by enamel on the crown and cementum on the root, surrounding the entire pulp. By weight, dentin is composed of 70% hydroxylapatite (a mineral, also known as hydroxyapatite), 20% organic material, and 10% water.
Dentin Structural Units include Dentinal Tubules (DT) and Odontoblastic Processes as well as Peritubular and Intertubular Dentin. Here are details about each of these structural units:
Dentinal Tubules (DT) and Odontoblastic Processes
Dentin contains microscopic channels called dentinal tubules, which radiate outward from the pulp to the exterior cementum or enamel border. These tubules extend from the dentin enamel junction (DEJ) in the crown area or the dentinocemental junction (DCJ) in the root area to the outer wall of the pulp. They contain fluid and cellular structures (Tome’s fiber). Dentinal tubules have a larger diameter near the pulpal cavity (3-4 µm) and a smaller diameter at their outer ends (1 µm). The terminal part of the DT branches into 2-3 branches near the DEJ, resulting in an increased number of DTs in this area. Additionally, there are lateral branches of DTs called canaliculi.
The course of dentinal tubules is curved, resembling an ‘S’ shape known as primary curvature. This configuration indicates the course taken by odontoblasts during dentinogenesis, starting at right angles from the pulpal surface and ending perpendicular to the DEJ. In the root and in the area of the incisal edge or cusps, the dentinal tubules are almost straight. The tubules are farther apart in the peripheral layers and more closely packed near the pulp.
Peritubular and Intertubular Dentin
A 1 µm thick sheath of peritubular dentin surrounds each tubule (about 0.75 µm near the DEJ and 0.4 µm near the pulp). Peritubular dentin is highly calcified and about 40% more calcified than adjacent intertubular dentin. Intertubular dentin is located between the dentinal tubules and forms the majority of the dentin. It is less mineralized than peritubular dentin and consists of a coarse network of collagen fibers in which apatite crystals are deposited.
Incremental Lines in Dentin
Incremental lines in dentin are microscopic growth lines that can be observed within the dentin structure of a tooth. These lines represent the daily, rhythmic deposition of dentin by odontoblasts, the cells responsible for dentin formation. Incremental lines provide valuable information about the growth pattern, rate, and history of dentin formation. There are several types of incremental lines in dentin:
- Imbrication or von Ebner lines: These fine lines run at right angles to the dentinal tubules and their course indicates the growth pattern of the dentin. The distance between the lines corresponds to the daily rate of apposition, which in the crown varies from 4-8 µm and decreases as root formation progresse.
- Counter lines of Owens: These hypocalcified lines can be seen as accentuated few lines in longitudinal ground sections. These lines arise due to disturbances in the dentin matrix and mineralizing process.
- Neonatal lines: These distinct lines separate prenatal and postnatal dentin and are mostly found in deciduous and first permanent molars. These lines result from incomplete calcification due to metabolic disturbances at the time of birth, which are related to abrupt changes in environment and nutrition.
- Interglobular dentin: Sometimes, mineralization of dentin begins in small globular areas that normally fuse to form a uniformly calcified dentin layer. If fusion does not take place, hypo-mineralized regions (in which only the primary mineralization phase occurs) remain between the globules, termed interglobular dentin.
In addition to the various types of incremental lines, dentin may also display other structural features, such as Tomes’ granular layer, which is located in the root dentin near the cementum. It is believed that Tomes’ granular layer represents an interference with the mineralization of the entire surface layer of root dentin before cementum formation begins.
Overall, incremental lines in dentin offer valuable insights into the growth and development of teeth, as well as potential clues about an individual’s life history and health status.
Dentin and Pulp Germ Layer
Dentin is a hard, mineralized tissue that forms the bulk of the tooth structure, located beneath the enamel and cementum. It is produced by specialized cells called odontoblasts, which originate from the mesoderm germ layer.
Similarly, the pulp is a soft, vascular tissue that fills the central cavity of the tooth and contains nerves and blood vessels. The pulp also derives from the mesoderm germ layer, specifically from the dental papilla, a mass of mesenchymal cells that gives rise to both dentin and pulp during tooth development.
In summary, both dentin and pulp are derived from the mesoderm germ layer during embryonic development.
Dentin and the Oral Microbiome
The oral microbiome is a complex ecosystem of microorganisms, including bacteria, viruses, fungi, and other microbes, that inhabit the oral cavity. These microorganisms play a crucial role in maintaining oral health and can also contribute to the development of various oral conditions, such as dental caries and periodontal disease.
A balanced oral microbiome contributes to oral health by promoting a stable and diverse microbial community that works synergistically to maintain a healthy oral environment. This balance is essential for preventing the growth of harmful bacteria and the development of oral diseases. Here are some ways in which a balanced oral microbiome supports oral health:
- Inhibition of pathogenic bacteria: Beneficial microbes in the oral cavity can compete with harmful bacteria for nutrients and binding sites on oral surfaces, preventing the colonization and growth of pathogenic bacteria that can cause dental caries, periodontal disease, and other oral infections.
- Production of antimicrobial substances: Some beneficial oral bacteria produce antimicrobial substances, such as bacteriocins and hydrogen peroxide, which can inhibit the growth of harmful bacteria, thus helping maintain a healthy oral environment.
- Neutralization of acids: Certain oral bacteria can metabolize acids produced by other bacteria, which helps maintain a balanced pH in the oral cavity. This is crucial for preventing the demineralization of tooth enamel and dentin, which can lead to dental caries.
- Regulation of the immune system: A balanced oral microbiome can help modulate the host’s immune response, preventing excessive inflammation that can damage oral tissues and contribute to the development of periodontal disease.
- Maintenance of oral mucosal barriers: A healthy oral microbiome supports the integrity of the oral mucosal barriers, which serve as a physical barrier against harmful bacteria and other pathogens.
- Promotion of oral tissue repair: Some beneficial oral bacteria can produce factors that promote the healing and repair of oral tissues, such as stimulating the production of collagen and other extracellular matrix components.
Dentin, the hard, mineralized tissue that forms the bulk of the tooth structure beneath the enamel and cementum, interacts with the oral microbiome in multiple ways. In healthy teeth, the dentin is protected by a layer of enamel on the crown and cementum on the root, making it relatively resistant to bacterial invasion. However, when these protective layers are compromised, such as by dental caries, tooth decay, or gum recession, the dentin can become exposed to oral bacteria and their by-products. This exposure can have several consequences:
- Breakdown of dentin matrix components: Oral bacteria produce acids and enzymes that can break down the organic and inorganic components of the dentin matrix. This process weakens the dentin structure and can lead to the formation of cavities or other defects.
- Inflammatory and immune responses: The interaction between oral bacteria and dentin can activate local inflammatory and immune responses. These responses are essential for limiting the spread of bacterial infection, but they can also cause collateral damage to the surrounding dental tissues, contributing to the progression of dental caries and periodontal disease.
- Pulp involvement: As bacteria penetrate the dentin, they can reach the pulp, a soft, vascular tissue that fills the central cavity of the tooth. Bacterial invasion of the pulp can lead to pulpitis, an inflammation of the pulp that can cause severe tooth pain and may eventually require root canal treatment or tooth extraction.
- Biofilm formation: Oral bacteria can form biofilms on exposed dentin surfaces. Biofilms are structured communities of bacteria encased in a self-produced extracellular matrix. They are more resistant to antimicrobial agents and mechanical removal than planktonic bacteria, making them particularly challenging to treat and control.
- Direct dentin degradation: Some studies have suggested that certain species of oral bacteria, such as Streptococcus mutans, may be able to directly degrade dentin, further contributing to the progression of dental caries.
Maintaining a balanced oral microbiome is essential for preserving dentin and overall oral health. Good oral hygiene practices, such as regular tooth brushing, flossing, and dental check-ups, can help control the growth of harmful bacteria and minimize the risk of dentin exposure and dental disease. In addition, certain treatments, such as fluoride application and dental sealants, can help strengthen and protect the dentin from bacterial invasion.
In summary: The relationship between dentin and the oral microbiome is complex and multifaceted. On one hand, the oral microbiome plays an important role in maintaining oral health, on the other hand, it can also contribute to the development of dental disease, particularly when dentin is exposed to oral bacteria and their by-products.